
CMS LIVING KIDNEY DONOR TRANSPLANT FACILITATOR PROGRAM PROPOSAL
Proposal Overview:
Americans with End Stage Kidney Disease (ESKD) have two options: dialysis, which is an expensive, time consuming and difficult treatment, or a kidney transplant. Yet, there is a significant shortage in America of kidneys available for transplant. With the kidney transplant waitlist including nearly 100,000 Americans, the number of deceased donors has increased more than 100% over the past 20 years but the number of living donors has not increased at all. To date, however, Medicare has not been leveraged to expand living kidney donation. To address this, the upcoming Medicare Physician Fee Schedule rule can be enhanced to establish a Living Donation Facilitator Program for advanced chronic kidney disease patients and potential living donors. This reform to existing Medicare policy would likely save thousands of lives and billions of dollars.
The Problem
Almost One Million Americans Have Kidney Disease: The National Institutes of Health reports that as of 2023 about 808,000 Americans were living with End-Stage Kidney Disease (ESKD).1 There are two primary treatments for the disease – dialysis or kidney transplant. As of December 31, 2024, 517,421 Americans are on dialysis.2 As of April 2025, 90,780 patients are on the kidney transplant waitlist.3 With only 27,000 transplants occurring in 2024, the waitlist is growing faster than the number of individuals receiving a transplant. Sadly, the United States now ranks 22nd in the world in transplants for people on dialysis.4
Medicare Spending on Kidney Disease Is Very High and Rising: Medicare spends a massive amount to treat ESKD patients on dialysis. The National Kidney Foundation reports that Medicare each year spends more than $130 billion (24% of overall spending) on patients with kidney disease and ESKD, which affects 1% of Medicare beneficiaries and accounts for 7% of total Medicare spend.5 Similarly, the NIH estimates that in 2021, 13.5% of the approximately 23.9 million Medicare fee for service beneficiaries over 66 years old years had a diagnosis of Chronic Kidney Disease (which includes ESKD), accounting for nearly one-quarter (24.1%) of total Medicare spending – an estimated $76.8 billion dollars. Within that group, approximately two thirds of the cost ($52.3B in 2021) was spent on care for ESKD beneficiaries.
Kidney Transplant Is the Optimal Treatment – Both from a Health and Fiscal Perspective: Kidney transplant is the “optimal treatment” for those facing or on dialysis. “Although not a cure for kidney disease, a transplant can help a person live longer with a dramatic improvement in quality of life. On average, patients experience 14 to 16 years of function from a kidney from a living kidney donor, while few people survive more than a decade on dialysis”6 The health benefits of transplant are further enhanced by the cost savings. A recent private study, using Congressional Budget Office scoring conventions, has estimated that each kidney transplant saves Medicare $800,000 over ten years.7 Doubling the number of new living donor transplants over the next decade would reduce Medicare spending by $6.6 billion.
Deceased Donor Kidneys are Rising but Living Donor Rates Are Stagnant: There are two sources for kidney transplants: kidneys donated by deceased donors, and those donated by living donors. Living donor organs are preferrable for two reasons: (1) there will never be sufficient deceased organs available to meet patient needs;8 and (2) living donor kidneys last nearly twice as long as deceased donor kidneys,9 producing far better recipient health outcomes and avoiding individuals returning to the waitlist for a second transplant. Indeed, a recent study just published in JAMA Network Open employing a decision-analytic model examined the impact of a 10% or 50% expansion of patients added to the waiting list and concluded that approximately 2800 additional kidneys would need to become available to maintain current waiting times for the lower estimate while an additional 11,000 kidneys would need to be available in the case of a 50% expansion. The authors concluded that a reduction in the nonuse rate for deceased donor kidneys is simply inadequate and that efforts to increase deceased and living donation would be necessary to successfully enable an expansion of the waiting list.10
It should also be noted that living donation resulting in a living donor kidney transplant affords the most realistic opportunity for a pre-emptive kidney transplant. This means receiving a kidney transplant prior to requiring dialysis, not only resulting in the best survival and quality of life with complete avoidance of dialysis but also the most significant cost savings. This avoids the dramatic costs associated with the several months leading up to the initiation of dialysis along with the first year following the initiation of dialysis. These costs have been estimated at nearly $15,000 per month in the 60 days leading up to dialysis, persisting for almost 12 months following the initiation on dialysis.11
Unfortunately, even though living donation has been proven to be safe, living donation rates have stagnated, if not declined, over the past 20 years. Data from the Organ Procurement Transplant Network (OPTN), created by Congress to facilitate more transplants, documents that over the past twenty years deceased donation has increased by more than 100%, while living donation has stagnated.

One reason for this stagnation is that Medicare regulations work against advancing living donation, rather than aiding those with ESKD and advanced CKD in identifying living donors and assisting those potential living donors in pursuing the complex and costly process of kidney donation. As a result, for every 100 potential living donors who volunteer and complete the initial screening questionnaire, seven may successfully donate a kidney.12
The Importance of Living Donor Facilitation
Numerous clinical studies have demonstrated that transplant facilitator interventions could materially increase living donor transplantation. Providing a “transplant facilitator” to the potential recipient to help identify a living donor and providing a similar “transplant facilitator” to a potential donor to help them complete the complex pre-donation and donation process would materially increase the number of living donations from today’s stagnant rates.13 It should also be noted that a planned living donor kidney transplant allows for a scheduled surgery maximizing the transplant hospital’s OR schedule and greatly benefiting both the recipient and donor as they can take advantage of a planned surgery.
Assisting Potential Recipients in Identifying Donors: Expecting ESKD patients to find living donors on their own is often unrealistic. Studies, however, have shown that dialysis patients working with a “transplant facilitator” to arm them with the language to make the ask, identify potential donors, and in some cases even initiate the outreach for the potential recipient, significantly increases the likelihood that a living donor can be found.14 By intervening with those needing a transplant at an early stage, these issues can be overcome inexpensively and efficiently.15 The Johns Hopkins “Champions” program reported a massive increase in recipients identifying living donors following the assistance of a facilitator:
Current educational modalities or interventions do not adequately meet the needs of patients who would like to pursue and identify live donors. Education alone is not sufficient to decrease the anxiety and fear associated with approaching potential donors. In this trial, LDCs successfully helped increase comfort and decrease concerns associated with approaching a live donor. A dramatic proportion of participants (almost 50%) identified live donors, compared with matched controls for whom no live donors were identified.16
Providing those eligible for transplant with a facilitator using the Hopkins protocols to assist in identifying living donors would add a massive number of new transplants to the system at trivial cost, driving huge savings.
Assisting Potential Donors in Navigating the System: Similarly, giving individuals who volunteer to be considered for living donation a “facilitator” to help them through the extensive medical testing and eventual surgery has also been shown to multiply the prospects of living donation. In one study at the University of Alabama Birmingham (UAB):
[i] implementation of a [Living Donor Facilitator] Program was associated with a 9-fold increased likelihood of living donor screenings and a 7-fold increased likelihood of having an approved living kidney donor among program participants compared to standard of care.”17
Again, providing a potential donor with a facilitator would cost a trivial amount, for massive returns. As noted above, today 93 of every 100 potential living donors willing to be screened never make it to donation. Adding facilitators could radically change that figure, and increase living donation 7 times, so that 49 of the 100 candidates actually complete the donation.
A conservative estimate using the data from the University of Alabama at Birmingham suggests that implementing these modest changes by utilizing transplant facilitators would double the number of living donors over the next two years to between 12,000 -13,000 per year. This would immediately improve outcomes, while reducing the wait list and Medicare spending. Additional studies have examined the numerous steps in which a care facilitator could assist a living donor in the lengthy and complicated process of the decision to donate, the successful completion of the screening and evaluation process, the living donation surgery, immediate post-donation care and then long-term care.18
The successful identification of a potential living kidney donor and the completion of the process to become a successful living kidney donor is challenging and as noted above, currently leads to less than 10% of identified donors donating a kidney. Care facilitators can significantly alter this dynamic with minimal additional cost to the healthcare system and dramatic savings for the healthcare system following successful living donor kidney transplant.
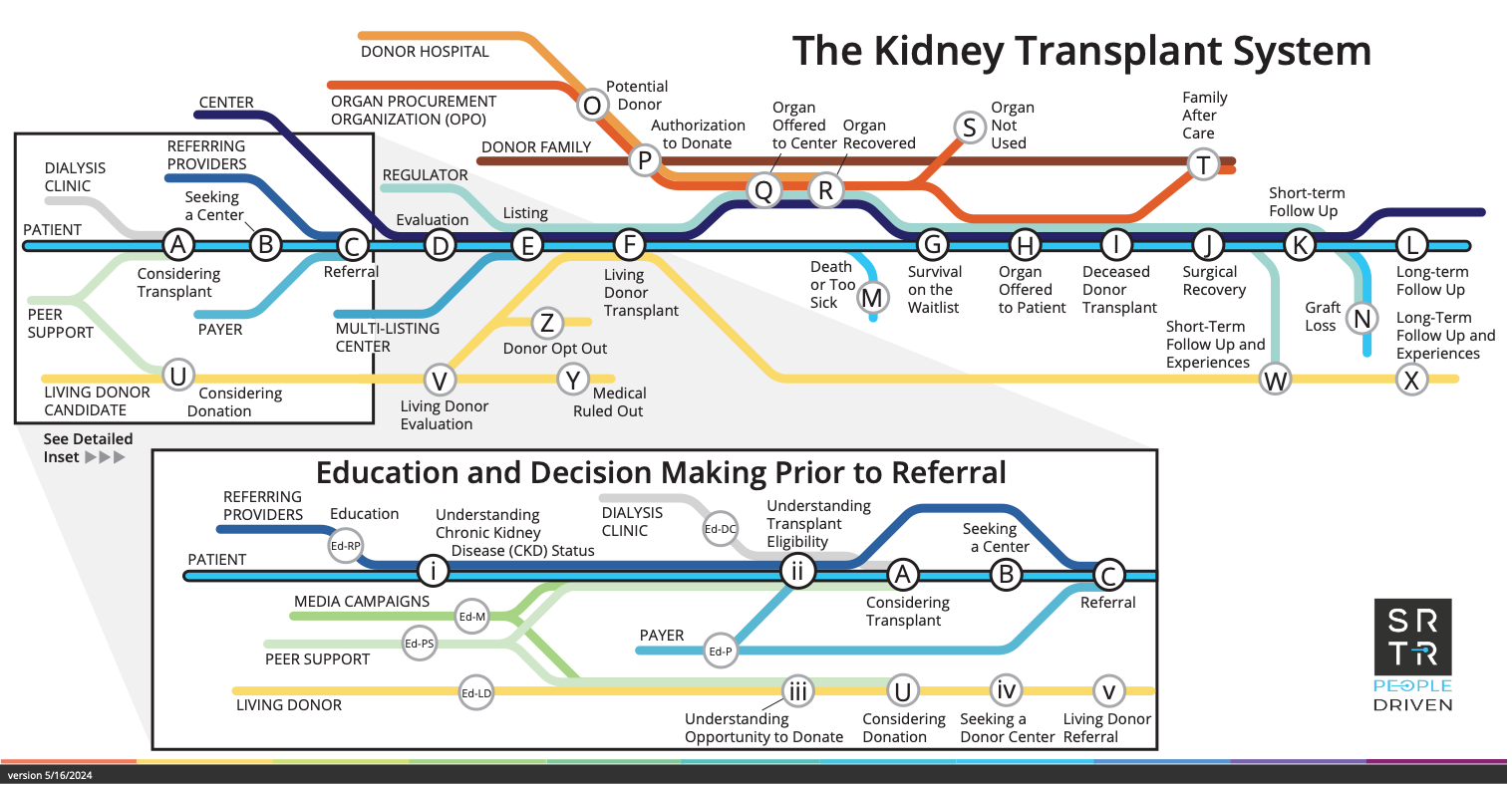
The attached road map from the Scientific Registry for Transplant Recipients identifies the complex steps that a potential donor must complete prior to even being referred to a transplant center, which is then followed by a lengthy pre/post transplant focused series of steps. This process can be initially supported by a nephrology practice-based dacilitator and then by a transplant center-based facilitator following referral. Under a partnership between nephrology practices and transplant centers, the full donation process could also be supported by one facilitator. Action is needed, and needed now, to implement the policy changes that will remove living donation barriers.
The Medicare Fee Schedule Solution
The 2024 Medicare Physician Fee Schedule Rule for the first time included a direct Medicare reimbursement program for “Principal Illness Navigators,” or PINs, principally in the oncology, cardiac and respiratory arenas. Under this program, physicians could be reimbursed for hiring facilitators to provide individualized help to the patient (and caregiver, if applicable) to access necessary and timely care, especially when the landscape is complex and delaying care can have severe consequences. The Final Rule did clarify that patients with chronic kidney disease could be included, although it was not specific to transplant. The final rule did not explicitly include nor exclude reimbursement for the facilitation of living donors both in identification of these individuals by the patient with CKD and to assist the living donor in the successful completion of the complicated and multi-step evaluation process.19 Although there appears to be very gradual recognition of the inclusion of chronic kidney care related reimbursement for the use of these PINs in the Medicare Physician Fee Schedule, the majority of providers involved in the advanced CKD/ESKD space are also simply unaware of these new provisions.
This existing Principal Illness Navigator program could be clarified to create a specialized Living Kidney Donor Transplant Facilitator program for ESKD and advanced CKD patients who are potential transplant recipients and for prospective living donors who are willing to donate a kidney to help them. More specifically, these changes to the Physician Fee Schedule (PFS) could include:
- Clarify patient facilitation for kidney transplant recipients as viable reimbursable activity, removing any room for interpretation, to include assistance in finding a living donor.
- Establish patient facilitation for living donors as viable reimbursable activity.
- Establish that potential living donors are not responsible for co-pays.
- Increase existing program’s payment rate (1 RVU, or $32.35 per hour (2025 rate) of navigator services) to a 2 RVU payment structure to support the specialized services needed for living donation facilitation. The payment could be increased as follows:
- G0023 – PIN services by certified or trained auxiliary personnel under the direction of a physician or other practitioner, 60 minutes per calendar month.
- G0024 – PIN services, additional 30 minutes per calendar month
With these four modest changes, nephrologists and physicians associated with transplant programs could hire qualified transplant facilitators to assist both recipients and living donors through the program, increasing the number of living donor transplants, improving health outcomes, and saving Medicare significant sums.
Key Impact and Savings
These key proposed changes to the Medicare Physician Fee Schedule could be effectuated either by legislation or CMS led rulemaking. The proposed 2026 Physician Fee Schedule is expected to be released sometime in late June with a 60-day public comment period and the release of a final rule in the fall. Irrespective, the projected impact, as determined by a recent private study, is significant.
A recent private study, using Congressional Budget Office scoring conventions, has estimated that each kidney transplant saves Medicare $800,000 over ten years. Doubling the number of new living donor transplants over the next decade from the current level of just over 6,000 living donor kidney transplants performed each year to 12,000 – 13,000 living donor kidney transplants each year would reduce Medicare spending by $6.6 billion.18 This would be expected to result in almost 40,000 kidney transplants performed annually given the expected continued increase in deceased donor kidney transplants. If one considers the possibility of genetically modified pig to human kidney transplants by that time, the possibility of a receiving a timely lifesaving kidney transplant for all Americans who need one is a real possibility.
Most advances in healthcare result in an improved quality of life along with longer expected survival; however, at an increased cost. This proposal represents one of the few examples in which there is an immediate positive impact on quality of life and survival alongside a significant long-term reduction in existing healthcare expenditures.
Implementing these modest changes likely would double the number of living donors over the next decade, improving outcomes, reducing the wait list, and reducing Medicare spending. Action is needed, and needed now, to implement the policy changes that will remove living donation barriers.
Annotations:
2 https://esrdnetworks.org/resources-news/national-esrd-census-data/
3 https://optn.transplant.hrsa.gov/data/dashboards-metrics/
5 https://www.kidney.org/get-involved/advocate/legislative-priorities/federal-investment
6 Medicare Program; Alternative Payment Model Updates and the Increasing Organ Transplant Access (IOTA) Model, 89 Fed. Reg. 96280, 96294 (December 4, 2024)
7 The Moran Company, The Living Organ Volunteer Engagement (LOVE) Act: Fiscal Implications (March 15, 2024), available from author
8 Matas AJ, Montgomery RA, Schold JD. The Organ Shortage Continues to Be a Crisis for Patients With End-stage Kidney Disease. JAMA Surg. 2023 Aug 1;158(8):787-788. doi: 10.1001/jamasurg.2023.0526.
9 National Kidney Foundation, Becoming a Donor https://www.kidney.org/kidney-topics/becoming-livingdonor#:~:text=Lasts%20longer%20%2D%20On%20average%2C%20a,away%20than%20deceased%20donor%20kidneys.
10 JAMANetworkOpen.2025;8(3):e251665.doi:10.1001/jamanetworkopen.2025.1665
11 League RJ, Eliason P, McDevitt RC, Roberts JW, Wong H. Assessment of Spending for Patients Initiating Dialysis Care.
12 Holin LK, Schold JD, Arrigain S, Poggio ED, Sedor JR, O’Toole JF, Augustine JJ, Wee AC, Huml AM. Characteristics of Potential and Actual Living Kidney Donors: A Single-center Experience. Transplantation. 2023 Apr 1;107(4):941-951. doi: 10.1097/TP.0000000000004357. Epub 2022 Nov 21. PMID: 36476994.
13 Federal law and regulation requires transplant programs to have adequate support for living donors, 42 C.F.R. § 482.94, including having on staff an “independent living donor advocate team.” 42 C.F.R. § 482.98(d). While transplant hospitals do an excellent job at assisting the living donor through the surgical process, there is no federal program or Medicare regulation addressing living donation before a living donor arrives at a transplant hospital
14 Garonzik-Wang JM, Berger JC, Ros RL, Kucirka LM, Deshpande NA, Boyarsky BJ, Montgomery RA, Hall EC, James NT, Segev DL. Live donor champion: finding live kidney donors by separating the advocate from the patient. Transplantation. 2012 Jun 15;93(11):1147-50. doi: 10.1097/TP.0b013e31824e75a5. PMID: 22461037; PMCID: PMC3374007
15 See also Killian AC, Carter AJ, Reed RD, Shelton BA, Qu H, McLeod MC, Orandi BJ, Cannon RM, Anderson D, MacLennan PA, Kumar V, Hanaway M, Locke JE. Greater community vulnerability is associated with poor living donor navigator program fidelity. Surgery. 2022 Sep;172(3):997-1004. doi: 10.1016/j.surg.2022.04.033. Epub 2022 Jul 10. PMID: 35831221; PMCID: PMC9633042 (“The Living Donor Navigator (LDN) Program helps patients with end stage kidney disease identify living kidney donors and helps living donors navigate the complex evaluation process. LDN participants have demonstrated a 9-fold increased likelihood of donor screening and 7-fold increased likelihood of donor approval compared to nonparticipants”).
16 Id.
17 Locke, J., et al. Enhanced Advocacy and Health Systems Training through Patient Navigation Increases Access to Living Donor Kidney Transplantation, Transplantation. 2020 Jan; 104(1): 122–129. doi: 10.1097/TP.0000000000002732.
18 The Moran Company, The Living Organ Volunteer Engagement (LOVE) Act: Fiscal Implications (March 15, 2024), available from author.
19 Loban K, Fadel E, Nugus P, Przybylak-Brouillard, Badenoch H, Robert JT, Bugeja a, Gill J, Fortin MC, Rodriguez C, Sandal S. Living Kidney Donors” Health Care Needs, Experiences, and Perspectives Across Their Entire Donation Trajectory: a Semistructured, in-depth Interview Study. Kidney International. (2024) 105, 251-258 doi.org/10.1016/.kint.2023.11.004
